AN OVERVIEW OF DIAGNOSTIC TREADMILL EXERCISE TESTING
Dr John McLeish Revised November 2014
1. INDICATIONS FOR EXERCISE TESTING
Exercise testing remains, despite some limitations, a highly valuable and relatively inexpensive non-invasive diagnostic procedure in Cardiology. It has many indications which may be divided into several groups, viz:-
(1) DIAGNOSIS
- diagnosis of suspected coronary artery disease (CAD) in the presence of typical symptoms
- diagnosis of atypical symptoms
- diagnosis in patients with presyncope or syncope during or following exertion
- evaluation of patients with multiple risk factors (particularly diabetes mellitus) wishing to undertake vigorous exercise programmes
(2) FUNCTIONAL EVALUATION OF PATIENTS WITH KNOWN CAD
- submaximal test 3 to 7 days after acute myocardial infarction (AMI) for risk stratification
- symptom-limited test 14 to 21 days after AMI
- functional evaluation following percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG)
- evaluation of medical therapy in patients with CAD
- evaluation of exercise capacity as part of a cardiac rehabilitation programme
- evaluation of patients with stenotic or regurgitant valve lesions (not performed in patients with severe symptomatic aortic stenosis)
- functional evaluation of patients with hypertrophic cardiomyopathy (impaired BP response associated with adverse prognosis)
- functional evaluation of individuals with PVD (eg with symptoms of claudication)
(3) MISCELLANEOUS
- preoperative evaluation before noncardiac surgery, to assess risk of perioperative ischaemia
- assessment of ventricular arrhythmias, in conjunction with Holter monitoring and electrophysiological studies
- evaluation of HR response to exercise in patients with rate-adaptive pacemakers
The test is not recommended for:-
- routine screening for coronary artery disease in asymptomatic individuals with minimal
(eg pilots, train drivers) may impact public safety
- diagnosis of CAD where the ECG precludes accurate interpretation of ST changes
- Left bundle branch block (LBBB)
- Preexcitation (WPW ECG abnormality)
- Digitalis therapy
- LV hypertrophy with pre-existing ST depression >1mm
- ventricular paced rhythm
- routine evaluation of exercise capacity
2. EXERCISE PHYSIOLOGY, EXERCISE PROTOCOLS & EXERCISE DURATION
Exercise testing measures an individual’s metabolic workload in terms of the maximum respiratory oxygen uptake (V̇O2max) achieved, using units called METs (metabolic equivalents). One MET is defined as the V̇O2 for a seated 70 kg, 40 year-old male at rest, and is equivalent to an oxygen uptake of 3.5ml/min/kg of body weight. The use of a standardized unit allows comparison of workloads achieved using different exercise protocols.
Standardized tables of workloads achieved (in METs) may overstate actual V̇O2max achieved under several circumstances, including:-
- allowing the patient to hold onto the treadmill handrail may overstate workload by up to 20% (however use of the handrail is necessary for safety reasons in nearly all middle-aged or elderly patients referred for diagnostic testing)
- where the patient has not achieved steady-state (normally attained 60-120 seconds into a particular stage of an exercise protocol)
- in the elderly
- in the obese
Fitness levels in sedentary individuals are very low in comparison to persons who exercise regularly, who may have similar fitness to sedentary persons who are 30 or more years younger. In sedentary individuals V̇O2max decreases by approximately 10% per decade; by contrast studies of masters athletes who train regularly have shown a much slower fall in V̇O2max (5% or less per decade) with some individuals who train consistently actually showing increases in V̇O2max over 10 or more years.
In general in any age group women will have lower V̇O2max than men (equating approximately to half to one stage of the Bruce Protocol), due to several factors which include lower lean body mass and muscle mass, decreased heart and lung volumes, lower haemoglobin and generally lower levels of physical activity.
During exercise vagal tone is withdrawn (associated with increased HR); systolic BP increases (diastolic BP does not generally change significantly and may decrease due to exercise-induced vasodilation) and catecholamine release is associated with increased HR and ventricular contractility. Skeletal, coronary and cerebral circulation increases. Oxygen extraction may increase by threefold and cardiac output may increase by four- to sixfold.
Maximum HR may be predicted by the formula 220 – age in years (SD 10 to 12 bpm). A maximum HR achieved that is 10% or more below the predicted value is generally described as a blunted HR response while one 10% or more above the predicted value is considered to be supraphysiological.
EXERCISE PROTOCOLS
The most commonly used treadmill protocol for diagnostic testing is the Bruce Protocol, which in its standard format has seven (7) 3-minute stages of increasing speed and gradient which are summarised in the table below. Completion of the Bruce Protocol requires exceptional fitness and is rarely achieved except by athletes. Other protocols used include the De Busk Submaximal Protocol, commonly performed on post-MI patients prior to discharge from hospital, the De Busk Maximal Protocol, occasionally used in younger post-MI patients who have had a small and/or uncomplicated (eg non-Q-wave) MI, and the Naughton Protocol which starts at a very low workload and progresses in small increments of exertion at 2 minute intervals and may be suitable for frail or elderly patients
BRUCE PROTOCOL (3-minute stages)
|
|
STAGE
1 2 3 4 5 6 7 |
SPEED (kph)
2.7 4.0 5.4 6.7 8.0 8.8 9.6 |
GRADIENT (%)
10 12 14 16 18 20 22 |
APPROX METs
4.5 7.0 10.0 13.0 15.0 17.0 19.0 |
CUMULATIVE DISTANCE (metres)
135 335 605 940 1340 1780 2260 |
|
Following exercise the patient is routinely monitored for up to 6 minutes in a seated position to allow recovery and to exclude late ischaemic ST changes (which may occasionally be seen only in the recovery phase); where a test has been positive monitoring is continued until ischaemic ST changes have returned to baseline.
EXERCISE DURATION
The exercise duration achieved on a treadmill test has important prognostic implications, and an exercise test should be routinely performed prior to coronary angiography. The ability to achieve 10 METs or more (completion of Stage III of Bruce Protocol or higher) is normally associated with a good prognosis regardless of the anatomical extent of coronary artery disease. Conversely in a study by Weiner et al in 1984 patients unable to complete Stage I of the Bruce Protocol and with 1mm or more ST depression during exercise had an annual mortality of 5 per cent. It has long been known that following an acute myocardial infarction the inability to achieve 5 METs predicts a more serious prognosis; while conversely the ability to achieve 5 or 6 METs with a normal ECG and normal BP response is associated with a 1 year mortality of 1 to 2 percent. The achievement of a high workload suggests the absence of clinically significant coronary stenoses.
More recently both in patients with CAD and in the general population studies indicating a significant link between fitness and mortality rates have created much interest. In a landmark study published in 2002 Myers and colleagues reported on their study of 6,213 men referred for treadmill exercise testing and followed for a mean of 6.2 years. The patients were divided into two major groups: those with cardiovascular disease and those without, and were further divided into quintiles of exercise capacity. At the end of the study period those individuals in the least fit quintile (both for subjects with and without cardiovascular disease) had a greater than 4 times risk of death from all causes compared to the most fit subjects, and each 1 MET increase in exercise capacity conferred a 12 percent improvement in survival. The authors concluded that exercise capacity was a more powerful predictor of mortality among men than any other risk factor for cardiovascular disease.
An individual’s exercise capacity may be affected by many variables, including age, gender, weight, muscle mass, activity levels, genetic factors and the presence or otherwise of coexisting cardiovascular (eg valvular disease, cardiomyopathy), pulmonary (eg asthma, COPD), or other disease (eg anaemia, peripheral vascular disease, joint pain, intercurrent infection, etc); consequently it is difficult to design studies which provide meaningful data on average fitness levels for individuals within any age group. It is however useful for patients and their medical practitioners to have an indication of how the individual compares to others of their gender and age group. While not based on a formal clinical trial I believe the table below, reflecting my own practice, provides an approximation of the treadmill time (Bruce Protocol, with the patient holding the treadmill bar) that might be expected for individuals of normal weight (BMI <25) without cardiovascular, respiratory or peripheral vascular disease, and undertaking moderate regular physical activity, but not training for competitive sports.
EXERCISE DURATION
The exercise duration achieved on a treadmill test has important prognostic implications, and an exercise test should be routinely performed prior to coronary angiography. The ability to achieve 10 METs or more (completion of Stage III of Bruce Protocol or higher) is normally associated with a good prognosis regardless of the anatomical extent of coronary artery disease. Conversely in a study by Weiner et al in 1984 patients unable to complete Stage I of the Bruce Protocol and with 1mm or more ST depression during exercise had an annual mortality of 5 per cent. It has long been known that following an acute myocardial infarction the inability to achieve 5 METs predicts a more serious prognosis; while conversely the ability to achieve 5 or 6 METs with a normal ECG and normal BP response is associated with a 1 year mortality of 1 to 2 percent. The achievement of a high workload suggests the absence of clinically significant coronary stenoses.
More recently both in patients with CAD and in the general population studies indicating a significant link between fitness and mortality rates have created much interest. In a landmark study published in 2002 Myers and colleagues reported on their study of 6,213 men referred for treadmill exercise testing and followed for a mean of 6.2 years. The patients were divided into two major groups: those with cardiovascular disease and those without, and were further divided into quintiles of exercise capacity. At the end of the study period those individuals in the least fit quintile (both for subjects with and without cardiovascular disease) had a greater than 4 times risk of death from all causes compared to the most fit subjects, and each 1 MET increase in exercise capacity conferred a 12 percent improvement in survival. The authors concluded that exercise capacity was a more powerful predictor of mortality among men than any other risk factor for cardiovascular disease.
An individual’s exercise capacity may be affected by many variables, including age, gender, weight, muscle mass, activity levels, genetic factors and the presence or otherwise of coexisting cardiovascular (eg valvular disease, cardiomyopathy), pulmonary (eg asthma, COPD), or other disease (eg anaemia, peripheral vascular disease, joint pain, intercurrent infection, etc); consequently it is difficult to design studies which provide meaningful data on average fitness levels for individuals within any age group. It is however useful for patients and their medical practitioners to have an indication of how the individual compares to others of their gender and age group. While not based on a formal clinical trial I believe the table below, reflecting my own practice, provides an approximation of the treadmill time (Bruce Protocol, with the patient holding the treadmill bar) that might be expected for individuals of normal weight (BMI <25) without cardiovascular, respiratory or peripheral vascular disease, and undertaking moderate regular physical activity, but not training for competitive sports.
|
|
Age (Years)
30 40 50 60 70 80 |
Males (minutes)
15 - 16½ 13½ - 15 12 - 13½ 10½ - 12 9 - 10½ 7½ - 9 |
Females (minutes)
13½ - 15 12 - 13½ 10½ - 12 9 - 10½ 7½ - 9 6 - 7½ |
|
Actual treadmill times achieved will of course vary widely depending on the factors mentioned above, of which obesity and a sedentary lifestyle have a greater impact than age in determining fitness levels.
3. DIAGNOSTIC CONSIDERATIONS
In assessing the value of a diagnostic test the concepts of sensitivity and specificity must be considered as well as the likelihood of disease in the individual being studied (Bayes’ Theorem)
Sensitivity of an exercise test is defined as the percentage of patients with coronary artery disease who have an abnormal test (i.e. the more sensitive a test the more likely an individual with coronary artery disease will have an abnormal test). Sensitivity = TP/(TP + FN)
Specificity of the test is the percentage of patients without coronary artery disease who have a normal test (i.e. the more specific a test, the more likely an individual with normal coronary arteries with have a normal test). Specificity = TN/(TN + FP)
[TP = true positive; TN = true negative; FP = false positive; FN = false negative]
Test accuracy is the percentage of true test results (i.e. true positive plus true negative) divided by the total number of tests performed.
Sensitivity and specificity are inversely related, i.e. increasing the diagnostic cut-off of ST depression for a positive test from 1mm to 2mm increases the specificity of the test but reduces its sensitivity.
The pre-test likelihood of disease (ie risk factors) should always be considered together with the test results (ST depression etc) in determining the post-test probability of disease.
The exercise test is less sensitive in the presence of a previous extensive anterior Q-wave MI.
Bayes’ Theorem states that the significance of a test result relates not only to the sensitivity and specificity of the test but also the prevalence of disease in the population being studied, thus the yield of exercise testing will be high in older males with multiple risk factors for coronary artery disease but the test will be relatively unreliable in studying young or middle-aged women who have a much lower incidence of disease and frequently demonstrate false-positive ST changes.
The sensitivity of stress testing varies with the extent of disease, viz sensitivity in single vessel disease has been reported as varying from 25-71% (with exercise-induced ST depression most common in patients with left anterior descending disease, followed by right coronary artery disease and circumflex disease) with a mean sensitivity of 81% for multivessel disease and 86% for left main disease.
In assessing the probability of a positive test several parameters are considered; including:-
The presence of an abnormal exercise ECG in asymptomatic middle aged men is said to range from 5 to 12% (with a nine-fold increase in cardiac events such as angina, AMI or death in individuals with an abnormal test over 5 years of follow-up; approximately 1 in 4 men will have a cardiac event) and asymptomatic middle-aged females have an abnormal test result in 20 to 30% of cases. Accordingly the test is much less accurate in asymptomatic middle-aged women, a group with a low incidence of CAD.
Typically the presence of angina and ST segment changes during exercise (arbitrarily 1mm or more of slow upsloping, horizontal or downsloping depression at 60 to 80msec past the J point) have been considered the most important parameters for diagnosis. Rapid upsloping ST depression of 1 to 1.5mm at the J point is a common ECG finding at high levels of exertion (particularly in women) and is non-diagnostic.
Note the following:-
In the absence of diagnostic ST changes during exercise testing the following additional features increase the probability of ischaemia being present if the patient:-
ST segment changes during exercise may be difficult to interpret in several clinical situations and in such cases SPECT (single-photon emission computed tomography) radionuclide scans or stress echocardiography may assist with the diagnosis; however where there is a strong clinical suspicion of CAD coronary angiography will often be the most appropriate investigation to evaluate regional myocardial perfusion, particularly where there is a strong clinical suspicion of underlying coronary artery disease. In stress echocardiography the development of wall motion abnormalities (or worsening of existing wall motion abnormalities) with exercise are indicative of exercise-induced myocardial ischaemia, as well as LV cavity dilation or impairment of global systolic function. These changes may not be present if exercise has been inadequate or if the patient is on beta-blockers. It should be emphasized that these expensive procedures should not be requested unless there is a clear clinical indication.
4. THE ST SEGMENT IN SPECIFIC CLINICAL SITUATIONS
The following clinical situations may impact on the interpretation of ST changes during exercise and accordingly the accuracy of the test result:
1) Women False positive ST changes (usually rapid upsloping depression) are commonly seen in young or middle-aged females, a group which has a low incidence of IHD. These changes have been attributed to increased catecholamine release in women during exercise causing coronary vasoconstriction
2) Digitalis
ST changes with exercise cannot be interpreted accurately in patients on digitalis; resting ST depression will generally increase with exertion and digitalis effect may become manifest with exercise even if absent at rest. Digitalis-induced ST changes may persist for as long as two weeks following cessation of the drug. Digitalis may increase ischaemic ST changes during exercise, particularly in the elderly. The absence of ST changes during exercise in a patient taking digitalis is regarded as a valid negative test
3) Left Ventricular Hypertrophy
In patients with voltage criteria for LVH ST depression may occur with exercise and may be non-diagnostic, whether or not resting ST changes are present
4) Hypertension
Individuals with significant or long-standing hypertension may show ST/T changes on the resting ECG; the mechanism for this is believed to be subendocardial ischaemia (LV ‘strain’ pattern) representing a physiological imbalance between myocardial oxygen supply and demand, and may be present in the absence of coronary atherosclerosis. Such changes commonly increase with exercise and are non-diagnostic. False-positive ST changes may also be seen during exercise in hypertensive patients in the absence of resting repolarisation abnormalities
5) Left Bundle Branch Block and Right Bundle Branch Block
Abnormal repolarisation manifested by resting ST depression and T wave inversion is seen normally in LBBB in leads where the dominant deflection is a tall R wave (ST elevation is seen in leads where the dominant deflection is a deep S wave) and this depression routinely increases during exercise; as such the presence of LBBB precludes accurate evaluation of ST changes with exercise. Similarly in RBBB downsloping ST depression is frequently seen in leads V1-3 and may increase with exercise; however development of new ST depression in the inferolateral leads is likely to be due to ischaemia
6) Atrial Tachyarrhythmias
ST depression is commonly seen during atrial tachyarrhythmias with a very high heart rate (eg PAT, atrial fibrillation with a rapid ventricular response etc) and is caused by increased myocardial oxygen demands and ischaemia due to impaired filling of the coronary arteries; it is not diagnostic of coronary atherosclerosis
7) Wolff-Parkinson-White ECG Abnormality
Abnormal repolarisation manifested by ST depression is commonly seen in patients with preexcitation; changes in the ST segment with exercise are non-diagnostic. False-positive ST changes are common in patients with WPW ECG abnormality and occur in normally conducted beats as well as beats showing preexcitation
8) Early Repolarisation Variant
Physiological concave-upward ST elevation of 1mm or more is a common normal ECG finding in young men at rest (the so-called ‘early repolarisation variant’). It is associated with increased vagal tone and is most prominent during bradycardia. It may also sometimes be seen in middle-aged males. It is uncommon in females of any age and in elderly males, and normally returns to baseline during exercise; only depression of the ST segment below the isoelectric line is considered significant
9) Diuretics
Diuretic therapy may produce false positive ST segment and T wave changes in the absence of a low serum potassium; these changes may be reversed by potassium replacement and probably indicate an intracellular deficit
5. NONCORONARY CAUSES OF ST DEPRESSION
The following are clinically relevant causes of ‘false-positive’ ST depression (in several examples depression is due to ischaemia but is not necessarily associated with coronary artery disease, as discussed above):-
· drugs: digitalis, lithium, phenothiazines
· left ventricular hypertrophy; LV strain pattern
· severe hypertension (with or without voltage criteria for LVH)
· intraventricular conduction disturbances, including bundle branch block
· supraventricular tachyarrhythmias, including atrial fibrillation
· hypokalaemia
· hyperventilation
· preexcitation (WPW ECG abnormality)
· severe aortic stenosis
Less common causes include:-
· glucose load/post-prandial state
· cardiomyopathy
· anaemia
· hypoxia
· sudden excessive exercise in sedentary individuals
· severe volume overload: aortic or mitral regurgitation
· elevated right ventricular end-diastolic pressure eg pulmonary embolism; pulmonary stenosis
· mitral valve prolapse
6. THE STRONGLY POSITIVE STRESS TEST
The following features suggest significant coronary artery obstruction or the likelihood of multivessel disease:-
1) early onset of angina and/or ischaemic ST changes
2) ST depression of 2 or more mm and/or downsloping ST depression
3) Ischaemic changes in 5 or more leads
4) failure to achieve workload greater than 5 METS
5) failure to increase systolic BP greater than 120mm Hg or reproducible fall in BP of 10mm or more during exercise
6) ST changes persisting greater than 5 minutes in the recovery phase
7) ST elevation: generally signifies transmural ischaemia and more likely with severe proximal stenosis; may occur with coronary artery spasm
8) sustained or symptomatic ventricular tachycardia during test
7. RISKS & CONTRAINDICATIONS TO EXERCISE TESTING
Exercise testing is generally a very safe procedure with an overall mortality rate of less than 1 in 10,000 and a morbidity rate of adverse events (eg acute MI, nonfatal cardiac arrest) less than 5 in 10,000. The risk is greater in the early post-MI period (less than 4 weeks after infarction) and is approximately doubled if the exercise is symptom-limited as opposed to submaximal.
Patients who have had unstable angina should be free of rest pain or evidence of cardiac failure for 2-3 days before testing; similarly following infarction, submaximal exercise testing should be delayed for 3 to 5 days post-MI.
Risks may be further reduced if the following contraindications to exercise testing are observed:-
· <48hrs after acute myocardial infarction
· unstable angina with recent rest pain
· severe symptomatic aortic stenosis
· severe HOCM (hypertrophic obstructive cardiomyopathy)
· uncontrolled heart failure
· life-threatening arrhythmia
· high degree A-V block
· severe uncontrolled hypertension (greater than 220/120 at rest)
· acute myocarditis or pericarditis
· acute pulmonary embolus
· acute systemic illness eg influenza; fever
· severe anaemia
· metabolic disorders eg thyrotoxicosis
Relative contraindications to testing include mental or physical impairment or language difficulties.
Notwithstanding the fact that exercise testing should not be performed in individuals with severe symptomatic aortic stenosis, the test has been shown to be safe in patients with moderate to severe stenosis (valve area 0.5 to 1.5 sq cm). Findings such as an exaggerated HR response to low levels of exercise, hypotension or angina during exertion are indications for early valve replacement.
INDICATIONS FOR TERMINATING THE EXERCISE TEST
Safety is enhanced if the following criteria are observed for terminating exercise:-
· progressive fall in systolic BP (or > 10mm Hg fall from baseline)
· falling HR
· sustained ventricular or supraventricular tachycardia, or significantly increased ventricular ectopy
· development of AV block
· onset of significant angina; marked fatigue and/or dyspnoea
· ataxia (suggesting cerebral hypoperfusion) or significant lightheadedness or confusion
· cyanosis or pallor (due to poor peripheral perfusion)
· severe hypertension (SBP >250mm or DBP >120mm)
· ischaemic ST depression of 2mm or more or ischaemic ST elevation of 1mm or more in a non-Q-wave lead (NB: ST elevation is arrhythmogenic)
· bundle branch block where rhythm cannot be identified ie where VT cannot be excluded
· technical problems with ECG quality or measurement of BP
The test is always terminated if the patient requests that exercise stop.
Further Reading:
Braunwald: ‘Heart Disease’ 9th edition 2012 (Elsevier Saunders) : Chapter 14 Exercise Stress Testing by Bernard R Chaitman provides a comprehensive discussion of all clinical aspects of cardiac exercise testing and has been the major reference in preparing these notes
(see also Ch 15 Echocardiography and Ch17 Nuclear Cardiology)
3. DIAGNOSTIC CONSIDERATIONS
In assessing the value of a diagnostic test the concepts of sensitivity and specificity must be considered as well as the likelihood of disease in the individual being studied (Bayes’ Theorem)
Sensitivity of an exercise test is defined as the percentage of patients with coronary artery disease who have an abnormal test (i.e. the more sensitive a test the more likely an individual with coronary artery disease will have an abnormal test). Sensitivity = TP/(TP + FN)
Specificity of the test is the percentage of patients without coronary artery disease who have a normal test (i.e. the more specific a test, the more likely an individual with normal coronary arteries with have a normal test). Specificity = TN/(TN + FP)
[TP = true positive; TN = true negative; FP = false positive; FN = false negative]
Test accuracy is the percentage of true test results (i.e. true positive plus true negative) divided by the total number of tests performed.
Sensitivity and specificity are inversely related, i.e. increasing the diagnostic cut-off of ST depression for a positive test from 1mm to 2mm increases the specificity of the test but reduces its sensitivity.
The pre-test likelihood of disease (ie risk factors) should always be considered together with the test results (ST depression etc) in determining the post-test probability of disease.
The exercise test is less sensitive in the presence of a previous extensive anterior Q-wave MI.
Bayes’ Theorem states that the significance of a test result relates not only to the sensitivity and specificity of the test but also the prevalence of disease in the population being studied, thus the yield of exercise testing will be high in older males with multiple risk factors for coronary artery disease but the test will be relatively unreliable in studying young or middle-aged women who have a much lower incidence of disease and frequently demonstrate false-positive ST changes.
The sensitivity of stress testing varies with the extent of disease, viz sensitivity in single vessel disease has been reported as varying from 25-71% (with exercise-induced ST depression most common in patients with left anterior descending disease, followed by right coronary artery disease and circumflex disease) with a mean sensitivity of 81% for multivessel disease and 86% for left main disease.
In assessing the probability of a positive test several parameters are considered; including:-
- the presence of 1mm or more of slow upsloping, horizontal or downsloping ST depression
- the presence or absence of noncoronary causes of ST depression eg hypertension, LV hypertrophy
- the presence of angina
- age
- gender (and whether premenopausal or postmenopausal for women)
- atherosclerotic risk factors (eg smoking, diabetes mellitus, hypertension)
- increasing ventricular ectopic activity with increasing levels of exertion and ventricular arrhythmias in the early recovery period
- blunted HR response to exercise
The presence of an abnormal exercise ECG in asymptomatic middle aged men is said to range from 5 to 12% (with a nine-fold increase in cardiac events such as angina, AMI or death in individuals with an abnormal test over 5 years of follow-up; approximately 1 in 4 men will have a cardiac event) and asymptomatic middle-aged females have an abnormal test result in 20 to 30% of cases. Accordingly the test is much less accurate in asymptomatic middle-aged women, a group with a low incidence of CAD.
Typically the presence of angina and ST segment changes during exercise (arbitrarily 1mm or more of slow upsloping, horizontal or downsloping depression at 60 to 80msec past the J point) have been considered the most important parameters for diagnosis. Rapid upsloping ST depression of 1 to 1.5mm at the J point is a common ECG finding at high levels of exertion (particularly in women) and is non-diagnostic.
Note the following:-
- The degree of ST depression represents a continuum in which increasing depression suggests the likelihood of a more severe stenosis or multi-vessel disease
- In a small group of patients ischaemia is manifested by ST elevation rather than depression; this is believed to represent transmural ischaemia when it occurs in leads without Q waves; when present in leads with Q waves in post-AMI patients it is due to LV dyskinesis. Post-infarct ST elevation is seen relatively commonly in the early post-AMI period, particularly in patients with anterior infarcts, and its incidence decreases by 6 weeks post-infarct. It is generally associated with lower ejection fractions, more severe wall motion abnormalities and a poorer prognosis
- ST depression during exercise is generally seen in the inferolateral leads regardless of the actual site of the myocardial ischaemia (ie does not localize the artery involved), however the presence of ST elevation is relatively specific for the area of myocardial ischaemia and coronary artery involved
- Atrial repolarisation (Ta) waves, which are of opposite polarity to the P wave and normally hidden within the QRS complexes, may become visible at high levels of exertion and distort the ST segment. They are generally not visible by 1 minute recovery as heart rate slows following peak exertion but their superimposition on the ST segment may mimic ischaemia
- Where resting ST depression is present additional depression of 1 or more mm would be required to consider an ST change significant. If however resting depression of 1mm or more is present, further depression with exercise is unreliable in diagnosing coronary artery disease
- Diabetic individuals and the elderly often do not experience anginal pain in spite of ischaemic ST changes; conversely occasional patients may experience angina but not exhibit significant changes; this may occur for instance if global ischaemia is present (with anterior and posterior ST changes effectively cancelling each other out) or where the standard lead placement does not effectively ‘visualise’ the ischaemic area of myocardium (eg posterior ischaemia)
- Note that a positive exercise test cannot be diagnosed as a ‘false positive’ because coronary angiography fails to demonstrate lesions in the epicardial arteries; ischaemia may be present due to factors such as coronary artery spasm or decreased coronary vasodilator reserve
In the absence of diagnostic ST changes during exercise testing the following additional features increase the probability of ischaemia being present if the patient:-
- has impaired functional capacity (able to achieve only a small workload)
- has a fall in systolic BP with exercise or a flat BP response to increasing exertion suggesting left ventricular dysfunction (note however BP may fall following vigorous exertion due to vasodilation, particularly in unfit individuals)
- is unable to achieve predicted maximal HR (defined as 220 minus age in years, although wide individual variation occurs and maximum rates of 10% greater than or less than predicted value would not be considered abnormal).
- patients taking beta-blockers and calcium antagonists
- associated with physical deconditioning
- patients with sinus node dysfunction (sick sinus syndrome)
- submaximal exercise effort
- develops a third heart sound or basal rales following exercise, or
- shows increased ventricular ectopic activity with exertion (normally VEBs tend to be suppressed by sinus tachycardia during exercise), although this may be an unreliable marker for IHD
ST segment changes during exercise may be difficult to interpret in several clinical situations and in such cases SPECT (single-photon emission computed tomography) radionuclide scans or stress echocardiography may assist with the diagnosis; however where there is a strong clinical suspicion of CAD coronary angiography will often be the most appropriate investigation to evaluate regional myocardial perfusion, particularly where there is a strong clinical suspicion of underlying coronary artery disease. In stress echocardiography the development of wall motion abnormalities (or worsening of existing wall motion abnormalities) with exercise are indicative of exercise-induced myocardial ischaemia, as well as LV cavity dilation or impairment of global systolic function. These changes may not be present if exercise has been inadequate or if the patient is on beta-blockers. It should be emphasized that these expensive procedures should not be requested unless there is a clear clinical indication.
4. THE ST SEGMENT IN SPECIFIC CLINICAL SITUATIONS
The following clinical situations may impact on the interpretation of ST changes during exercise and accordingly the accuracy of the test result:
1) Women False positive ST changes (usually rapid upsloping depression) are commonly seen in young or middle-aged females, a group which has a low incidence of IHD. These changes have been attributed to increased catecholamine release in women during exercise causing coronary vasoconstriction
2) Digitalis
ST changes with exercise cannot be interpreted accurately in patients on digitalis; resting ST depression will generally increase with exertion and digitalis effect may become manifest with exercise even if absent at rest. Digitalis-induced ST changes may persist for as long as two weeks following cessation of the drug. Digitalis may increase ischaemic ST changes during exercise, particularly in the elderly. The absence of ST changes during exercise in a patient taking digitalis is regarded as a valid negative test
3) Left Ventricular Hypertrophy
In patients with voltage criteria for LVH ST depression may occur with exercise and may be non-diagnostic, whether or not resting ST changes are present
4) Hypertension
Individuals with significant or long-standing hypertension may show ST/T changes on the resting ECG; the mechanism for this is believed to be subendocardial ischaemia (LV ‘strain’ pattern) representing a physiological imbalance between myocardial oxygen supply and demand, and may be present in the absence of coronary atherosclerosis. Such changes commonly increase with exercise and are non-diagnostic. False-positive ST changes may also be seen during exercise in hypertensive patients in the absence of resting repolarisation abnormalities
5) Left Bundle Branch Block and Right Bundle Branch Block
Abnormal repolarisation manifested by resting ST depression and T wave inversion is seen normally in LBBB in leads where the dominant deflection is a tall R wave (ST elevation is seen in leads where the dominant deflection is a deep S wave) and this depression routinely increases during exercise; as such the presence of LBBB precludes accurate evaluation of ST changes with exercise. Similarly in RBBB downsloping ST depression is frequently seen in leads V1-3 and may increase with exercise; however development of new ST depression in the inferolateral leads is likely to be due to ischaemia
6) Atrial Tachyarrhythmias
ST depression is commonly seen during atrial tachyarrhythmias with a very high heart rate (eg PAT, atrial fibrillation with a rapid ventricular response etc) and is caused by increased myocardial oxygen demands and ischaemia due to impaired filling of the coronary arteries; it is not diagnostic of coronary atherosclerosis
7) Wolff-Parkinson-White ECG Abnormality
Abnormal repolarisation manifested by ST depression is commonly seen in patients with preexcitation; changes in the ST segment with exercise are non-diagnostic. False-positive ST changes are common in patients with WPW ECG abnormality and occur in normally conducted beats as well as beats showing preexcitation
8) Early Repolarisation Variant
Physiological concave-upward ST elevation of 1mm or more is a common normal ECG finding in young men at rest (the so-called ‘early repolarisation variant’). It is associated with increased vagal tone and is most prominent during bradycardia. It may also sometimes be seen in middle-aged males. It is uncommon in females of any age and in elderly males, and normally returns to baseline during exercise; only depression of the ST segment below the isoelectric line is considered significant
9) Diuretics
Diuretic therapy may produce false positive ST segment and T wave changes in the absence of a low serum potassium; these changes may be reversed by potassium replacement and probably indicate an intracellular deficit
5. NONCORONARY CAUSES OF ST DEPRESSION
The following are clinically relevant causes of ‘false-positive’ ST depression (in several examples depression is due to ischaemia but is not necessarily associated with coronary artery disease, as discussed above):-
· drugs: digitalis, lithium, phenothiazines
· left ventricular hypertrophy; LV strain pattern
· severe hypertension (with or without voltage criteria for LVH)
· intraventricular conduction disturbances, including bundle branch block
· supraventricular tachyarrhythmias, including atrial fibrillation
· hypokalaemia
· hyperventilation
· preexcitation (WPW ECG abnormality)
· severe aortic stenosis
Less common causes include:-
· glucose load/post-prandial state
· cardiomyopathy
· anaemia
· hypoxia
· sudden excessive exercise in sedentary individuals
· severe volume overload: aortic or mitral regurgitation
· elevated right ventricular end-diastolic pressure eg pulmonary embolism; pulmonary stenosis
· mitral valve prolapse
6. THE STRONGLY POSITIVE STRESS TEST
The following features suggest significant coronary artery obstruction or the likelihood of multivessel disease:-
1) early onset of angina and/or ischaemic ST changes
2) ST depression of 2 or more mm and/or downsloping ST depression
3) Ischaemic changes in 5 or more leads
4) failure to achieve workload greater than 5 METS
5) failure to increase systolic BP greater than 120mm Hg or reproducible fall in BP of 10mm or more during exercise
6) ST changes persisting greater than 5 minutes in the recovery phase
7) ST elevation: generally signifies transmural ischaemia and more likely with severe proximal stenosis; may occur with coronary artery spasm
8) sustained or symptomatic ventricular tachycardia during test
7. RISKS & CONTRAINDICATIONS TO EXERCISE TESTING
Exercise testing is generally a very safe procedure with an overall mortality rate of less than 1 in 10,000 and a morbidity rate of adverse events (eg acute MI, nonfatal cardiac arrest) less than 5 in 10,000. The risk is greater in the early post-MI period (less than 4 weeks after infarction) and is approximately doubled if the exercise is symptom-limited as opposed to submaximal.
Patients who have had unstable angina should be free of rest pain or evidence of cardiac failure for 2-3 days before testing; similarly following infarction, submaximal exercise testing should be delayed for 3 to 5 days post-MI.
Risks may be further reduced if the following contraindications to exercise testing are observed:-
· <48hrs after acute myocardial infarction
· unstable angina with recent rest pain
· severe symptomatic aortic stenosis
· severe HOCM (hypertrophic obstructive cardiomyopathy)
· uncontrolled heart failure
· life-threatening arrhythmia
· high degree A-V block
· severe uncontrolled hypertension (greater than 220/120 at rest)
· acute myocarditis or pericarditis
· acute pulmonary embolus
· acute systemic illness eg influenza; fever
· severe anaemia
· metabolic disorders eg thyrotoxicosis
Relative contraindications to testing include mental or physical impairment or language difficulties.
Notwithstanding the fact that exercise testing should not be performed in individuals with severe symptomatic aortic stenosis, the test has been shown to be safe in patients with moderate to severe stenosis (valve area 0.5 to 1.5 sq cm). Findings such as an exaggerated HR response to low levels of exercise, hypotension or angina during exertion are indications for early valve replacement.
INDICATIONS FOR TERMINATING THE EXERCISE TEST
Safety is enhanced if the following criteria are observed for terminating exercise:-
· progressive fall in systolic BP (or > 10mm Hg fall from baseline)
· falling HR
· sustained ventricular or supraventricular tachycardia, or significantly increased ventricular ectopy
· development of AV block
· onset of significant angina; marked fatigue and/or dyspnoea
· ataxia (suggesting cerebral hypoperfusion) or significant lightheadedness or confusion
· cyanosis or pallor (due to poor peripheral perfusion)
· severe hypertension (SBP >250mm or DBP >120mm)
· ischaemic ST depression of 2mm or more or ischaemic ST elevation of 1mm or more in a non-Q-wave lead (NB: ST elevation is arrhythmogenic)
· bundle branch block where rhythm cannot be identified ie where VT cannot be excluded
· technical problems with ECG quality or measurement of BP
The test is always terminated if the patient requests that exercise stop.
Further Reading:
Braunwald: ‘Heart Disease’ 9th edition 2012 (Elsevier Saunders) : Chapter 14 Exercise Stress Testing by Bernard R Chaitman provides a comprehensive discussion of all clinical aspects of cardiac exercise testing and has been the major reference in preparing these notes
(see also Ch 15 Echocardiography and Ch17 Nuclear Cardiology)
Fig.1
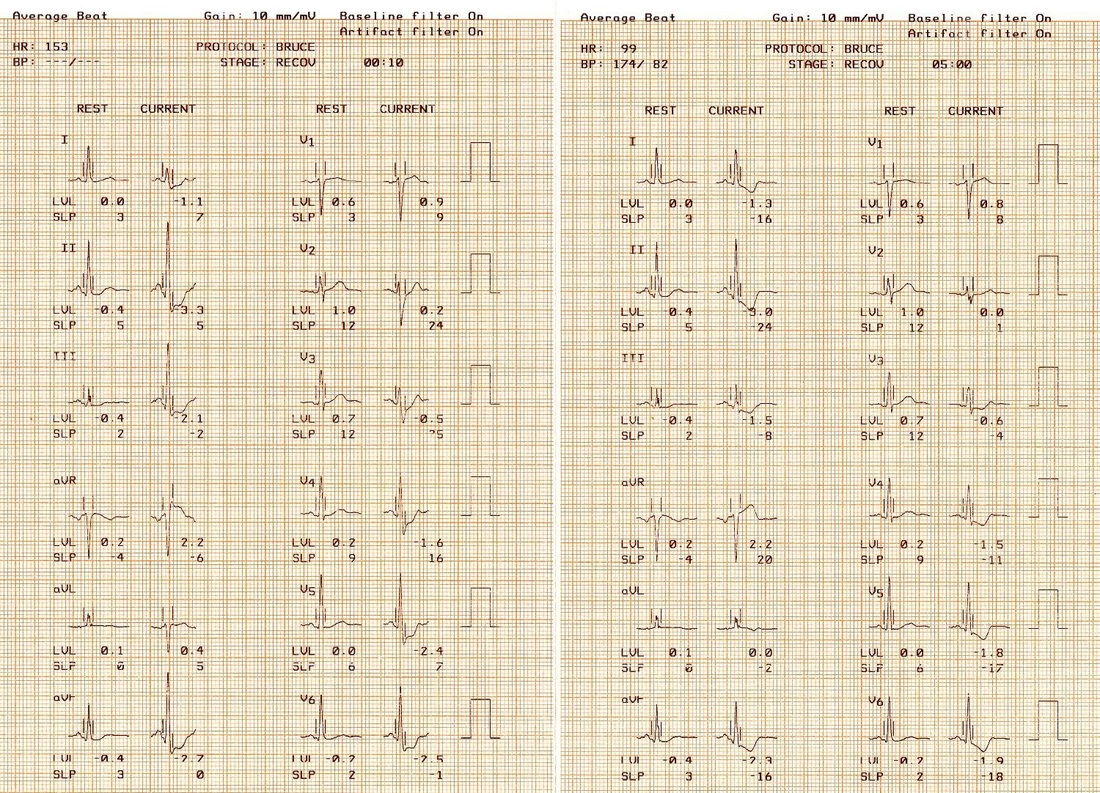
Fig.1 60 year old male with throat and upper retrosternal tightness on exertion. Exercise was ceased at 3:30 minutes (Bruce Protocol) because of up to 3mm ST depression consistent with ischaemia in the inferolateral leads; the patient experienced mild throat and chest discomfort from 3 minutes exercise. Widespread downsloping depression typical of ischaemia is seen at 5 minutes post-exercise. Angiography showed triple-vessel disease including 90% stenosis of the circumflex artery.
Fig.2a
|
Fig.2b |
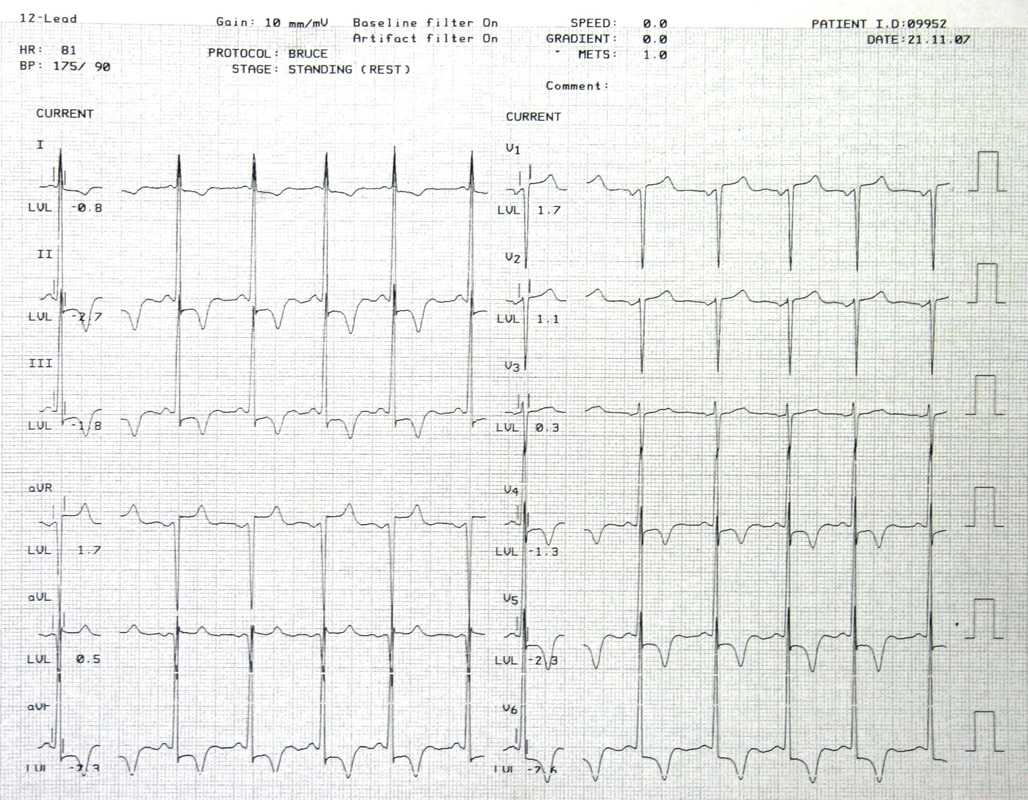
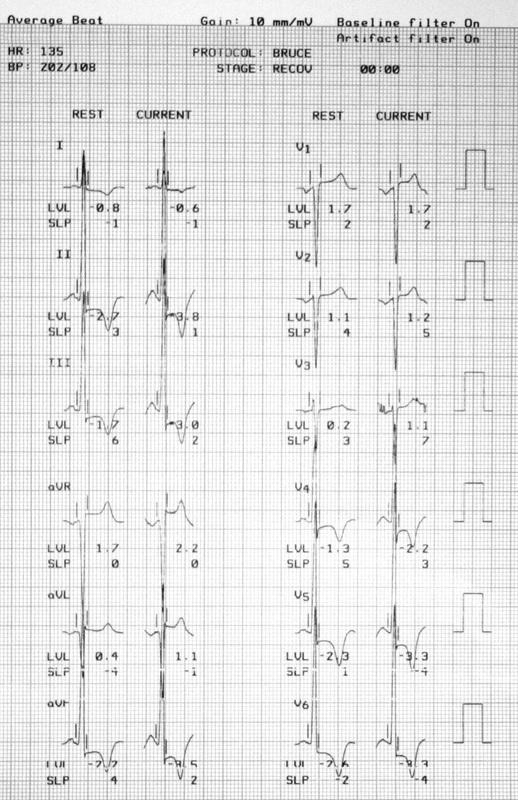
Fig 2a 12-lead resting ECG on a 59 year-
old female with atypical hypertrophic cardiomyopathy shows voltage criteria for LV hypertrophy (S in V2 + R in V5 approximately 50mm) with prominent ST depression and T inversion consistent with LV ‘strain’ pattern Fig 2b Computer-averaged QRS complexes at the end of exercise show additional ST depression of 1- 1.5mm inferolaterally compared to the resting ECG. The changes are non-diagnostic in the context of LV hypertrophy with prominent resting ST/T changes. The patient did not experience angina but was only able to achieve an extremely poor exercise workload (estimated less than 3 METS) due to marked dyspnoea and fatigue |
LIKE THIS ARTICLE? CLICK ON THE LINK BELOW TO DOWNLOAD AND PRINT
| Notes on Diagnostic Treadmill Exercise Testing |